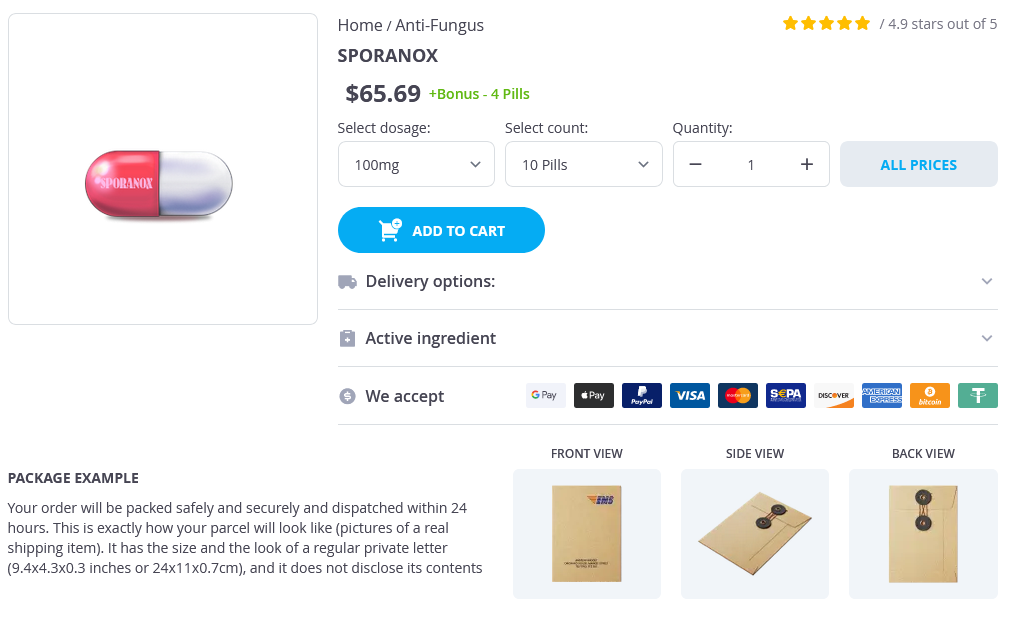
Sporanox
Sporanox
Sporanox dosages: 100 mg
Sporanox packs: 10 pills, 20 pills, 30 pills, 40 pills, 50 pills
In stock: 505
Only $4.66 per item
Description
The occasional presence of dysplasia suggests the possibility that these tumors may harbor a potential for malignant transformation into biliary cystadenocarcinomas fungus gnats damp 100 mg sporanox purchase with visa. Several noteworthy benign conditions must be considered in the differential diagnosis of obstructing biliary tract lesions. Primary sclerosing cholangitis is an idiopathic, premalignant disorder characterized by progressive biliary tract fibrosis whose cholangiographic appearance can mimic that of malignant biliary disease. Untreated, it can ultimately progress to cholestatic liver failure and cholangiocarcinoma. Mirizzi syndrome is an unusual benign condition resulting from a chronically impacted stone in the neck of the gallbladder that itself compresses the common bile duct or that over time induces sufficient pericholecystic inflammation to obstruct the adjacent common hepatic duct or common bile duct. Finally, another unusual benign process that can produce biliary tract obstruction is benign idiopathic focal stenosis, or the so-called malignant masquerade. Because of its propensity to involve the confluence of the hepatic ducts, this benign fibroproliferative disorder is often indistinguishable from cholangiocarcinoma without extensive surgical intervention. It may arise anywhere along the entire length of the biliary system; 40% to 60% develop in the hilum (hereafter referred to as hilar cholangiocarcinomas), 20% to 30% in the distal lower biliary tract (distal cholangiocarcinomas), 10% arise intrahepatically (the so-called peripheral or intrahepatic cholangiocarcinomas), and less than 10% develop in a diffuse or multifocal manner. Because of their anatomic differences, these subtypes are associated with distinct patterns of clinical presentation and require distinct strategies for surgical resection. As is the case with gallbladder cancer, the majority of patients with cholangiocarcinoma present with advanced disease that is not amenable to surgical resection; as a result, most patients die within 6 to 12 months of diagnosis from hepatic insufficiency or cholangitis. However, also like gallbladder cancer, improvements in diagnosis and surgical technique have given rise to new optimism in their management. Less common benign tumors include granular cell myoblastomas, neural tumors, endocrine tumors, and leiomyomas. Because they are found most frequently in the region of the ampulla of Vater or along the common bile duct, benign biliary tumors typically present with jaundice that is slowly progressive or intermittent in nature. Optimal treatment includes local excision with removal of a portion of the duct wall from which they originate because local recurrences have been reported after subtotal resection. Bile duct adenomas are benign intrahepatic tumors that are typically found incidentally at the time of laparoscopy or laparotomy. They often appear as welldemarcated white subcapsular lesions ranging from several millimeters to 1 or 2 cm in size. Histologically, they are characterized by numerous well-differentiated bile ductlike structures surrounded by a fibrous stroma. They are generally asymptomatic and have not been proven to be precancerous in nature. Biliary cystadenomas are unusual benign tumors often characterized by a multiloculated cystic appearance.
Hackmatack (Thuja). Sporanox.
- What is Thuja?
- Stimulating immune function, bronchitis, pneumonia, skin infections, herpes infections, nerve pain, strep throat, abortions, arthritis, joint pain, muscle aches, skin diseases, cancer, warts, and use as an insect repellent.
- How does Thuja work?
- Are there safety concerns?
- Are there any interactions with medications?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=97061
Cystoduodenostomy Cystoduodenostomy is rarely necessary antifungal for yeast infection sporanox 100mg purchase online, except when the pseudocyst is located at the pancreatic head and immediately abutting the duodenal wall. A longitudinal duodenotomy should be used to expose the medial wall of the duodenum. An aspirating needle can be used to identify the area of nearest apposition of the pseudocyst to the duodenal wall. When creating the 2- to 3-cm-long cystoduodenostomy, caution must be taken to avoid injury to the gastroduodenal artery, as well as the common bile duct or the main pancreatic duct. If those structures impede clear access to the pseudocyst from the medial duodenal wall, a cystojejunostomy may be preferable. Interrupted hemostatic sutures can be placed along the cystoduodenostomy if there is any bleeding from intervening pancreatic parenchyma. The lateral duodenotomy is then closed in one or two layers and a closed-suction drain may be placed per surgeon preference. Historically, a lateral side-to-side cystoduodenostomy has a high rate of morbidity and mortality related to anastomotic dehiscence and abscess formation, and therefore it should rarely (if ever) be performed. Nealon and Walser studied 103 patients with pseudocyst and chronic pancreatitis with a main pancreatic duct diameter of greater than 7 mm who received longitudinal pancreaticojejunostomy (Puestow procedure) alone for duct drainage or surgical cystojejunostomy combined with duct drainage. The wall of the pseudocyst must be mature and thick enough to hold suture for anastomosis, which is typically true more than 6 weeks after the initial appearance of the pseudocyst. In chronic pancreatitis, surgery for a pseudocyst may proceed as soon as any acute inflammation has subsided. Given the usual significant inflammation from the antecedent pancreatitis, dissection around the pseudocyst should be minimized whenever possible. If there is any concern about the possibility of a cystic neoplasm, a full-thickness biopsy of the cyst wall can be excised where the anastomosis will be performed and sent for immediate frozen section evaluation. Residual debris or necrotic material within the pseudocyst cavity should also be gently suctioned or debrided prior to anastomosis. Cystogastrostomy, Roux-en-Y cystojejunostomy, or cystoduodenostomy are options for internal drainage depending on the anatomic location of the pseudocyst. Especially in cases of giant pseudocysts, the anastomosis should be located to optimize dependent drainage of the pseudocyst. External drainage can result in a prolonged pancreaticocutaneous fistula, but may be necessary in emergent septic situations when a more definitive or extensive intervention is not prudent. Cystogastrostomy When the anterior pseudocyst wall is seen to be directly opposed to the posterior stomach wall from its location in the lesser sac, generally cystogastrostomy is the internal drainage procedure of choice.
Specifications/Details
The concept of "liver-related mortality" was introduced in an attempt to define those deaths likely due to the liver injury itself versus those related to associated trauma such as head injury fungus gnats definition generic sporanox 100 mg fast delivery. Although there are anecdotal reports of cholecystorrhaphy, the treatment of choice should be cholecystectomy. Attempts to repair even minor gallbladder injuries should generally be avoided because of the propensity for bile leakage and the risk of gallstone formation engendered by the inflammation around the suture used for repair. Typically, bleeding occurs several days to a few weeks after the injury and may be manifested by several clinical presentations. Hemobilia should be suspected in those who sustained recent liver injury with gastrointestinal bleeding and/ or jaundice. We do not recommend repair of these injuries at the initial operation but undertake hemorrhage control, drainage, and damage control. When the patient is resuscitated, we recommend defining the injury, then a planned return to the operating room with the company of an experienced hepatobiliary surgeon for reconstruction. Surgical treatment of injuries to the solid abdominal organs: a 50-year perspective from the Journal of Trauma. American Association for the Surgery of Trauma organ injury scale I: spleen, liver, and kidney, validation based on the National Trauma Data Bank. Early detection of hemoperitoneum by ultrasound examination of the right upper quadrant: a multicenter study. Western Trauma Association/ critical decisions in trauma: operative management of adult blunt hepatic trauma. Nonoperative management of blunt hepatic injury: an Eastern Association for the Surgery of Trauma practice management guideline. The swinging pendulum: a national perspective of nonoperative management in severe blunt liver injury. Concomitant hollow viscus injuries in patients with blunt hepatic and splenic injuries: an analysis of a National Trauma Registry database. Solid viscus injury predicts major hollow viscus injury in blunt abdominal trauma. The impact of a massive transfusion protocol (1: 1: 1) on major hepatic injuries: does it increase abdominal wall closure rates Implementation of a military-derived damage-control resuscitation strategy in a civilian trauma center decreases acute hypoxia in massively transfused patients. Interventional techniques are useful adjuncts in nonoperative management of hepatic injuries. Outcomes and complications of angioembolization for hepatic trauma: a systematic review of the literature.
Syndromes
- X-ray of the chest
- Wear compression stockings to decrease swelling. They gently squeeze your legs to move blood up your legs.
- Unconsciousness
- Your heart valve has been damaged by infection of the heart valve (endocarditis).
- Fever
- Burns of the food pipe (esophagus)
Related Products
Additional information:
Usage: q.3h.
Tags: 100mg sporanox visa, sporanox 100mg order with visa, purchase 100 mg sporanox with mastercard, buy sporanox 100mg otc
10 of 10
Votes: 199 votes
Total customer reviews: 199
Customer Reviews
Seruk, 35 years: They include both metastatic lesions with cystic degeneration and primary cystic tumors of the liver. Liver transplantation for hepatic angiocarcinoma has been associated with very high recurrence rates and is no longer recommended. Cystojejunostomy Cystojejunostomy is performed in a Roux-en-Y configuration (as compared to a loop configuration), thus yielding the advantage of keeping the flow of enteric contents away from the pseudocyst lumen.
Jorn, 54 years: Ideally, a total pancreatectomy would eliminate all risk, but this is a radical procedure that is associated with metabolic derangements and exocrine insufficiency. Most pancreatic adenocarcinomas arise from the head, neck, or uncinate process and are the predominant tumor pathology seen in this region. At 1, 3, and 5 years, overall survival rates were 88%, 69%, and 50%, respectively, whereas disease-free survival rates were 65%, 43%, and 43%, respectively.
Anog, 46 years: The pancreatic duct injury can be divided into proximal (at the head or neck, to the right side of the superior mesenteric vessels) and distal injuries (at the distal body and tail to the left side of the mesenteric vessels). By using a combination of gentle compression and palpation with one hand and sharp dissection with either scissors or a scalpel in conjunction with the use of copious amounts of saline-soaked sponges, one can usually carry out complete mobilization of the involved intestine. Determination of independent predictive factors for anastomotic leak: analysis of 682 intestinal anastomoses.
Sobota, 62 years: The dissection should be limited to the exposure needed to complete the planned procedure. However, these therapies are associated with significant side effects and have limited effectiveness. Options for bile duct decompression include surgical, percutaneous, and endoscopic methods.
Hengley, 41 years: Metal versus plastic for pancreatic pseudocyst drainage: clinical outcomes and success. Laparoscopic splenectomy: learning curve comparison between benign and malignant disease. Subsequently, the effect of repeated Kasai procedures is deleterious for liver transplantation.
Mannig, 47 years: Ligation of the hepatic artery and portal vein to one side causes the liver parenchyma to demarcate between the right and left liver. The main surgical dictum for treatment of the injuries should be to perform the minimal surgical intervention necessary to adequately treat the injury and accomplish these objectives. It is paramount to inspect the cut edge of the liver surface for any evidence of bleeding or bile leakage.
Gembak, 26 years: The glandular system is composed of the pituitary, parathyroids, paraganglia, and adrenal medulla. Disadvantages of this imaging modality include not only its invasive nature but also the resources necessary (angiography suite or operating room) to perform the test. The left hepatic vein, as well as branches from the middle hepatic vein and the left bile duct, can be controlled with a stapling device as they are encountered during the parenchymal transection.
-
Our Address
-
For Appointment
Mob.: +91-9810648331
Mob.: +91-9810647331
Landline: 011 45047331
Landline: 011 45647331
info@clinicviva.in -
Opening Hours
-
Get Direction